A lot of people are asking, How long will Covid-19 last?, Is the shutdown worth the cost? and Will we have shutdown, after shutdown? Nobody can answer the How long? question, at this stage. In this note, we ask what bounds we can put around that number, depending on the approaches we take.
The simplest answer to How long? is until we get a vaccine or treatment, or until we get to “herd immunity” or we get the reproduction number below one. There is a lot of promising work on vaccines, but a vaccine that works may be a year or 18 months away.
Herd immunity is the threshold level of immunity that a population needs to reach, for the disease to die away over time. It is the natural consequence of a pandemic that is left unchecked. The shortest path to herd immunity is to just let it rip; overwhelm the medical system by a factor of about 100 times what we have seen in Italy; and let hundreds of millions of people die needlessly. We want to be very clear: that isn’t something we would advocate.
The second and much preferred approach is to “flatten the curve” of new cases to within the capacity of the medical system. The numbers suggest that a flat curve, near capacity, is years long. But, without a vaccine, the real power, in terms of How long? and the economic pain, is likely to be in good habits and good systems, to get the reproduction number below one. To see why, it is useful to work through the numbers.
How long is the flat curve?
A lot has been said about slowing the rate of new infections, to a level within the capacity of the health system. First, let’s think about how long it takes to get through a flat curve, at the capacity level of critical care beds. That isn’t where we want to be, because we also want to have capacity for the usual illnesses. But a flat curve, at capacity level, gives a lower bound on the length of the flat curve. Below is a graph, from Statista, showing critical care beds by country. We are assuming critical care beds to mean a bed with a ventilator and medical staff with the required protection.

Image source: Statista.com
Those are the countries with the most beds, at various times during the decade before Covid-19. These beds are way below the level needed to manage an uncontrolled surge of Covid-19 cases, even in the best-equipped jurisdictions. We think Malaysia has a bit below 5 beds per 100,000 people. Let’s assume that countries can buy more ventilators, convert operating theatres into critical care beds, train or reassign medical staff, and provide protective equipment to be able to run them safely. Lombardy, in northern Italy, is reported to have doubled their critical care bed capacity in a short time. Let’s work with 10 beds per 100,000 as a round number.
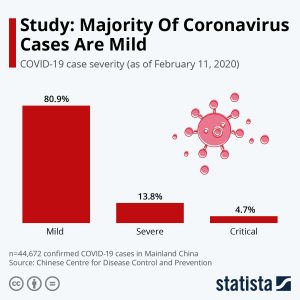
Image source: Statista.com
Suppose the goal is to give all critical patients (4.7 per 100, from the Statista chart below) access to a critical care bed. Let’s assume one critical care bed can serve three patients per month, or 36 per year. To provide for all of the patients who become critical, without being overwhelmed, would take 13 years (4.7% critical/0.36% per year).
‘Years’ is an order-of-magnitude estimate, meaning it is subject to a high degree of uncertainty. The critical rate is probably overestimated, because there is evidence of mild and asymptomatic cases, that haven’t been measured, in part for lack of testing capacity. A large number of uncounted mild cases implies a lower critical rate and a shorter time to get through the flat curve. If there is one unmeasured case out there for every measured one, then our 13 years is cut in half. On the other hand, we haven’t accounted for the 14% of severe cases, or for the critical care beds for other uses. Those imply a longer flat curve.
But so far, we have assumed that everyone gets the disease.
Herd immunity
Over time, the number of people who have recovered from the virus increases. The duration of immunity, after recovery, is uncertain. Evidence from SARS suggests at least a couple of years, but there isn’t good data for either SARS or MERS. Herd immunity is built on the idea that, as more people become immune, it becomes more difficult for the virus to spread. Immune people break the chain of infection. This shortens the flat curve. What share of the population needs to become immune for the spread to fall to a rate at which the disease dies out?
The answer varies according to the rate of spread. Epidemiologists talk about a “basic reproduction number”. The basic reproduction number is the average number of new cases caused by each new infection, left unchecked. Measles is very contagious: on average, one case spreads to 10 to 20 other people. For Covid-19, one case is estimated to lead to 1.5 to 4 new cases. Most early estimates are around 2 or 3. If you get infected with Covid-19, on average, you pass it on to 2-3 people, who each pass it on to 2-3 people, and so on. That basic reproduction rate is the rate of spread at the beginning of the outbreak, before measures are taken. As more people become immune, the actual rate of spread naturally falls, because immune people break the chain.
“Herd immunity” is the threshold that brings the actual reproductive number below one. For those who like equations, the herd immunity threshold is 1-1/R0, where R0 is the basic reproduction number. For measles the threshold is high: 90-95% of the population. For Covid-19, a reproduction number of 2.5 means a threshold of 60%. But it might be as big as 75% or as small as 33%. If the reproduction number is less than 1, the threshold is zero and disease fades away.
This is interesting for two reasons. First, we won’t all get Covid-19, although a lot of people fear we all will. Second, herd immunity reduces the “How long is the flat curve?” answer. It takes my all-of-us-get-it estimate of 13 years down to around 4 to 10 years. I am still hoping for a vaccine!
But that is still an incomplete story…
The power of habits: soap and kindness
The basic reproduction number is the rate of spread at the beginning of the outbreak before measures are taken. Handwashing, cleaning surfaces and physical distancing all reduce the rate of spread. If one case only spreads the virus to 1.5 others, on average, rather than three, then 9 years becomes 4 years.
There is evidence that asymptomatic cases are responsible for a significant share of the spread. Combined with evidence that droplets travel a long way, it is increasingly being recommended that we all wear a mask in public. Even homemade cloth ones are reported to protect others pretty well. That is kindness: I wear a mask for you; you wear a mask for me. Nike might make one saying, Just wear it. If masks reduce the reproduction number in half again, then the effective reproduction rate goes from 1.5 to 0.75.
At a reproduction number of one, all of the power of the exponential spread is gone. Below one, the power of the exponential curve starts to work in our favour: the virus dies away more and more quickly. Soap, masks and physical distancing are potentially powerful ways to reduce the reproduction number. These changes are cheap and can be aided by varying degrees of “nudge”, to make it easier for people to make responsible decisions.
Good systems
By identifying, tracing and isolating active cases, public health surveillance systems arrest the spread of the virus and further reduce the effective reproduction number. Technology is on our side. Testing is improving fast and online systems can aid self-reporting and contact tracing.
Travel has been a powerful way to spread the virus, both within and across borders. There are large externalities (costs to others) in the world of coronavirus, that make a case for systems to keep cross-border travel safe. Cross-border spread was disproportionally driven by the well-to-do travelling set, but disproportionately, the people who lost their jobs have been low-income service sector workers, with less access to healthcare. Countries are putting systems in place to prevent cross-border spread. The cost of international travel will be higher for a while, with testing and quarantine. (User pays. Take some work with you and book your quarantine online.) Korea is harnessing technology to make it easier. The reproduction number can be smaller again.
Large gatherings have provided environments where the reproduction number can go way up: one person can pass it directly to many. Parties, weddings, religious gatherings, business meetings, conferences and education have all been implicated. We are learning how to gather in ways that reduce reproduction rates – for example, online, in bigger spaces, in smaller groups, with masks and hand sanitizer provided and symptomatic people staying home. There is a lot of scope to reduce the reproduction number for gatherings.
Combine good habits with good systems, then even the high estimates of the basic reproduction number might be transformed into an effective reproduction number of less than one. How far the reproduction number can be reduced, once shutdowns stop, remains to be seen. But for sure, good health is good economics. The best way to save businesses and jobs is to maintain a reproduction number below one.
We work in higher education. Our challenge is to find safe ways to both travel and gather in groups. A reproduction number below one can be our guide. These changes are cheap, when compared to the alternative of shutdown and travel bans.
A new normal
When community spread accelerates, a stay at home order from the government is an effective way to reduce the reproduction number to well below one, But shutdowns are disastrous for the economy, at least in the short term: people lose their jobs and companies fail
Flatten the curve. Then what?

After stay-at-home orders are lifted, what might the new normal look like? If the reproduction number is above one, we risk repeated surges in cases and the risk of repeated shutdowns. If the reproduction number is below one, the disease dies out. At some point on the curve, we can propose a calibrated return to work, taking into account value (eg jobs), demographics (eg vulnerable groups), and the basic reproduction number for that activity. Low reproduction number activities might be eased first. Activities involving large groups, might come later, and only when they can show how the effective reproduction rate will be kept to below one. Then innovation will bloom, and the basic, cheap solutions like masks, soap and good systems become opportunities. Because of externalities, some activities will need to be regulated.
Thinking through the numbers provides a basis for thinking about exit strategies. Having a sense of the numbers, even if on a back-of-the-envelope basis, helps to give us perspective. It helps us to see the power of individual actions – we can take the power out of the Covid-19 curve. It helps us to see a light at the end of the dark tunnel of the heart-breaking news about areas that are well beyond care capacity, and people losing their jobs. It helps us to plan for a future, where the reproduction number is low enough to make stay-at-home orders isolated events. It helps us to plan for the worst, and to hope for a vaccine or effective treatment.
Professor Anella Munro is part of our Master of Central Banking team. Before joining ASB, she worked at the Reserve Bank of New Zealand, the Bank for International Settlements (Hong Kong office) and the Asian Development Bank. Her research interests are international macroeconomics, macro-prudential policy and international finance. She has a BSc in Electrical Engineering from MIT and a PhD in Economics from the University of Oxford.She can be contacted at anella.munro@asb.edu.my.

Professor Eli Remolona sits on the Board of Directors of the Bank of the Philippine Islands and is an Adviser to the Academy of Finance in Hong Kong. Prior to joining ASB, he had long careers at the Bank for International Settlements and the Federal Reserve Bank of New York. He has taught at Williams College, Columbia University and New York University and has been an Associate Editor of the International Journal of Central Banking since 2005. Eli holds a PhD in Economics from Stanford University. He can be contacted at eli.remonola@asb.edu.my.
If you are interested to know more about our exciting Master of Central Banking program click here.